Bakeri City, Pincode: 380015 Ahmedabad, Gujarat, India,
244 Madison Avenue, New York, United States
Our Client





Understanding the Functional Relationship Between Academic and Hospital Blocks
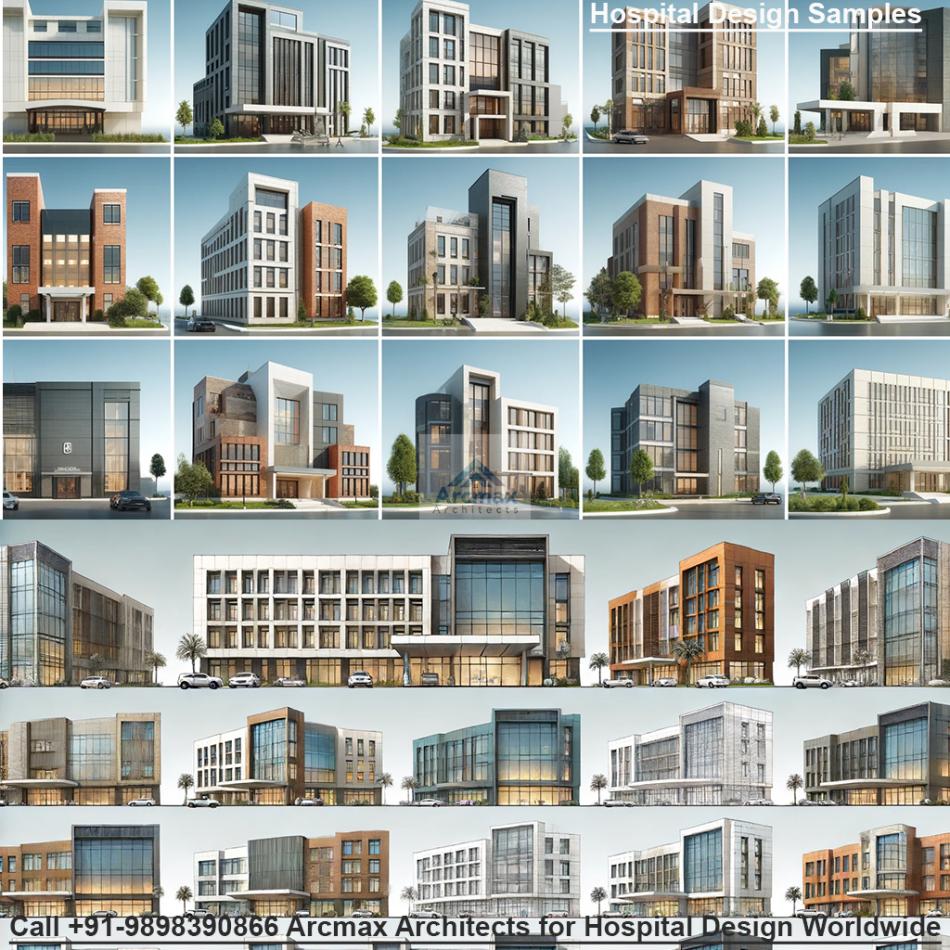
The Synergistic Spine: Understanding the Functional Relationship Between Academic and Hospital Blocks By Arcmax Architects, call +91-9898390866 for Hospital design and Planning worldwide
In the world of medical education and healthcare delivery, the architectural and operational relationship between the Academic Block (the medical college) and the Hospital Block (the teaching hospital) is not merely one of proximity; it is a dynamic, symbiotic connection that forms the very backbone of a successful institution. This functional relationship is the critical factor that transforms a collection of buildings into a cohesive "healthcare education ecosystem." It ensures that the journey from a student in a classroom to a clinician at a patient's bedside is seamless, efficient, and continuously reinforced.
Understanding this interconnection is to understand the philosophy of modern medical training. It’s about creating a physical environment where theory and practice are in constant dialogue, fostering a generation of physicians who are not just knowledgeable, but are also adept, empathetic, and collaborative from day one of their careers.
The Philosophical Foundation: From "Silos" to "Synergy"
Traditionally, medical colleges and hospitals could operate as separate "silos," with distinct administrations, cultures, and physical barriers. This model is obsolete. The contemporary paradigm is built on "translational integration"—the continuous, bidirectional flow of information and experience.
Theory Informs Practice: Knowledge from the classrooms and laboratories guides clinical reasoning and treatment decisions.
Practice Informs Theory: Unanswered questions and observations from the clinical wards feed back into the curriculum and spark new research.
The physical design of the campus is the primary enabler of this philosophy. It must intentionally break down barriers and create a "synergistic spine"—a network of pathways, both physical and digital, that bind the two blocks into a single, powerful entity.
The Physical Connectors: Weaving the Two Blocks Together
The first and most tangible layer of this relationship is the physical connectivity that allows for the effortless movement of people.
1. The Central Atrium and "Main Street" Concept:
Many modern facilities employ a grand central atrium or a "Main Street" corridor that serves as the primary artery. This space is more than a hallway; it's the social and intellectual heart of the institution. It connects the main entrance of the academic block to the hospital's public concourse, lined with cafes, bookshops, and collaboration nooks. Here, students grabbing coffee can overhear consultants discussing a complex case, and researchers can casually bump into clinical colleagues, fostering the informal exchanges that often lead to innovation.
2. Skybridges and Underground Tunnels:
Especially in multi-story complexes or climates with extremes, skybridges and subterranean tunnels are indispensable. They provide all-weather, secure, and efficient routes for the constant back-and-forth movement of students, residents, and faculty. A well-planned network ensures that a student can move from a lecture on cardiology in the academic block to observing a cardiac catheterization in the hospital's cardiology department within minutes, without ever stepping outside. This preserves the momentum of learning and reinforces theoretical concepts with immediate practical exposure.
3. Vertical Integration with Centralized Cores:
In vertically integrated designs, shared services are often stacked or placed in a central core. For instance, the Central Diagnostic Department (encompassing Radiology, Pathology, and Biochemistry) might be strategically located on a floor that is easily accessible from both the hospital's inpatient floors and the academic block's research labs. This allows medical students and researchers to access imaging and lab data for their studies while clinicians use the same facilities for patient diagnosis, creating a natural overlap of activity.
The Functional Integration: How Specific Spaces Interconnect
The true test of the relationship is how specific academic spaces interact with their clinical counterparts.
The Classroom to Clinical Department Link:
Scenario: A morning lecture in the academic block on "Neurological Assessment."
The Connection: The curriculum is deliberately structured so that this lecture is immediately followed by a scheduled clinical posting in the hospital's Department of Neurology. The physical proximity, enabled by the connectors mentioned above, allows students to directly apply the cranial nerve examination techniques they just learned on real patients under supervision. This "see one, do one, teach one" model is dramatically enhanced when the distance between "seeing" and "doing" is minimized.
The Laboratory to Bedside Link (Translational Research):
Scenario: A pharmacology lab in the academic block is researching a new anti-cancer drug.
The Connection: The laboratory is not isolated. Its location is chosen for its proximity to the hospital's Oncology Ward and Clinical Research Unit. This allows the basic scientists to easily collaborate with clinical oncologists. Patient tissue samples (handled ethically and with consent) can be transported securely to the lab for analysis. Conversely, promising compounds from the lab can be moved efficiently into early-phase clinical trials within the same campus. This "bench-to-bedside" pipeline is the holy grail of modern medicine and is entirely dependent on this functional integration.
The Simulation Center: The Ultimate Bridge:
The Simulation Center is arguably the most critical interfacing space. It is a hybrid entity, belonging wholly to neither the academic nor the hospital block but serving both.
Function for Academics: It is a safe, controlled environment for students to learn and practice procedures—from suturing to complex surgical simulations—on high-fidelity manikins before ever touching a patient.
Function for the Hospital: It serves as a training and credentialing hub for resident doctors and nursing staff. They can rehearse rare but high-stakes clinical scenarios, like cardiac arrest or difficult airway management, ensuring team proficiency and enhancing patient safety.
The Spatial Relationship: Its ideal location is physically between the two blocks or equally accessible from both. This symbolizes its role as the essential transitional zone, building student confidence and clinical competence in a risk-free environment.
Operational and Digital Synchronization
A seamless physical design is futile without synchronized operations and a robust digital backbone.
1. Unified Scheduling and Logistics:
The timetables of the academic block and the clinical postings in the hospital must be intricately coordinated. A centralized scheduling system ensures that when students are taught a module, their corresponding clinical rotations are aligned. Furthermore, logistical flows—such as the transport of anatomical specimens from the anatomy lab to the hospital's mortuary or the delivery of pharmaceuticals from research labs—require carefully planned service corridors that do not interfere with public or patient areas.
2. The Digital Nervous System:
Technology is the invisible web that binds the two blocks. A unified Electronic Medical Record (EMR) system, accessible from terminals in both the hospital wards and the academic libraries (with appropriate privacy controls), allows students to study real, anonymized patient cases as part of their curriculum. A integrated Learning Management System (LMS) delivers lecture notes, virtual microscopy slides, and clinical guidelines to students' devices, whether they are in a classroom or on a hospital round. Telemedicine suites in the hospital can also be used for remote teaching, allowing a specialist in the operating room to broadcast a procedure to an entire lecture hall.
The Human Element: Fostering a Collaborative Culture
Ultimately, the most sophisticated design is only a scaffold. The goal is to foster a culture of collaboration.
Shared Spaces: Designing shared spaces like faculty lounges, libraries, and cafeterias that are used by both academics and clinicians breaks down professional barriers and encourages interdisciplinary dialogue.
Interprofessional Education (IPE) Zones: Dedicated spaces designed for students of medicine, nursing, pharmacy, and physiotherapy to learn together mimic the team-based approach of modern clinical care, preparing them for real-world collaboration.
Conclusion: More Than the Sum of Its Parts
The functional relationship between the Academic Block and the Hospital Block is the defining characteristic of a world-class medical institution. It is a meticulously planned interplay of architecture, technology, operations, and culture. When executed successfully, the campus ceases to be perceived as two separate entities. Instead, it becomes a single, integrated learning health system where every corridor, every bridge, and every digital connection is purposefully designed to accelerate the transformation of a student into a healer, and a scientific discovery into a life-saving therapy. This synergistic spine ensures that the institution is perpetually evolving, learning, and delivering卓越的护理, truly becoming more than the sum of its parts.