Bakeri City, Pincode: 380015 Ahmedabad, Gujarat, India,
244 Madison Avenue, New York, United States
Our Client





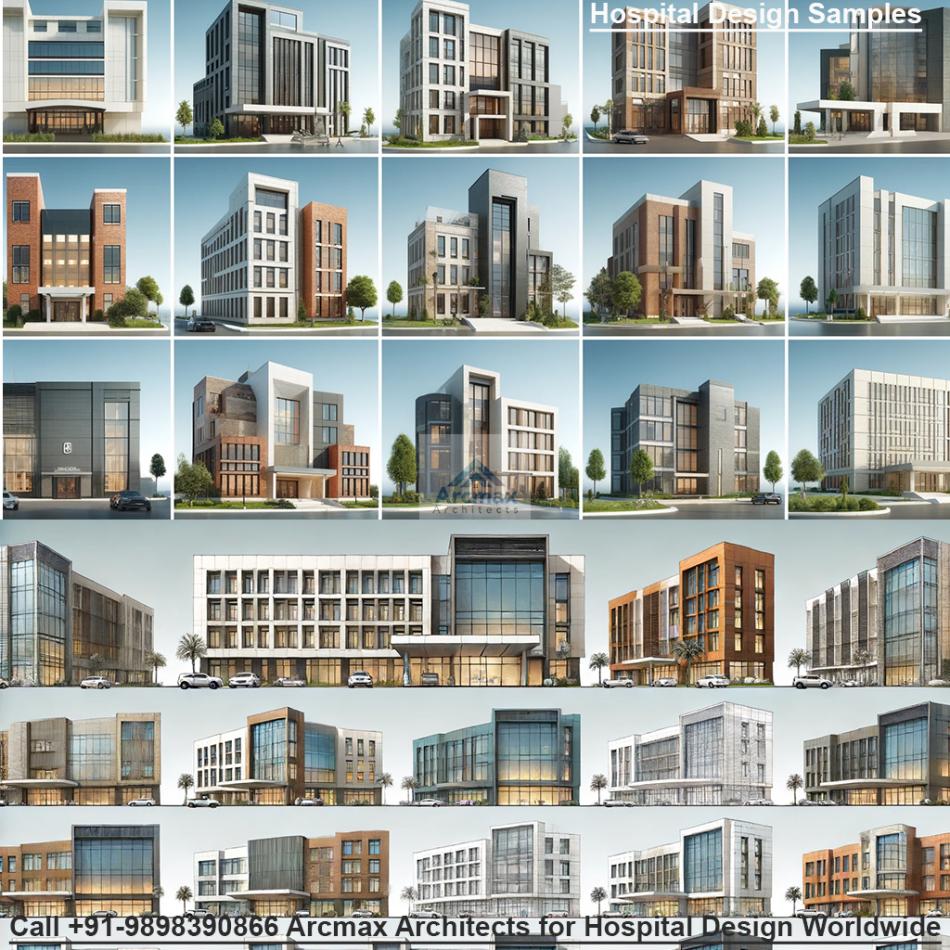
Infrastructure Requirements for a Teaching Hospital and Allied Facilities
The Anatomical Blueprint: Designing Infrastructure for a Modern Teaching Hospital and its Allied Facilities
A teaching hospital is far more than a place of healing; it is a living, breathing, three-dimensional textbook. It is a complex organism where the urgent, life-saving pulse of clinical care must synchronize perfectly with the deliberate, inquisitive rhythm of medical education and the innovative hum of research. Designing the infrastructure for such an institution is a monumental task that requires a deep understanding of workflow, human psychology, and the symbiotic relationship between practice and pedagogy. The ultimate goal is to create an environment that not only delivers卓越的 patient care but also actively fosters the development of future clinicians and accelerates medical discovery.
This intricate dance between care, teaching, and research is orchestrated within specific functional zones, each with its own unique requirements and critical connections to the whole.
1. The Emergency & Trauma Unit: The Beating Heart of Acute Care
The Emergency Department (ED) is the hospital's front line, a high-stakes, high-stress environment that demands an infrastructure designed for speed, adaptability, and resilience.
Infrastructure Core: The design must facilitate a clear "pit-resuscitation-zone" model. The central "pit" is for rapid triage and assessment of walk-in patients, surrounded by dedicated resuscitation bays for critical cases. These bays require in-room CT scanners, digital X-ray, and point-of-care ultrasound to minimize patient movement. Ample space is non-negotiable to accommodate large teams of students, residents, nurses, and consultants during a code.
Integration with Teaching: The ED is a premier teaching ground. This requires strategic design elements like:
Glass-walled bays that allow for visual supervision of multiple patients simultaneously by senior staff.
Decentralized workstations placed between bays to keep clinicians close to patients while documenting, enabling students to observe decision-making in real-time.
Adjacent simulation/debriefing rooms for immediately practicing or reviewing rare procedures or team dynamics after a critical case, solidifying the learning experience.
2. The Outpatient Department (OPD): The Gateway to Ambulatory Care
The OPD is the hospital's public face, handling a high volume of patients with diverse needs. Its infrastructure must prioritize efficiency, patient comfort, and clear wayfinding.
Infrastructure Core: The most effective model is a "clustered pod" layout. Instead of long, impersonal corridors, specialty clinics (e.g., Cardiology, Neurology, Orthopedics) are housed in their own self-contained pods. Each pod contains consultation rooms, a dedicated nursing station, minor procedure rooms, and patient waiting areas. This minimizes cross-traffic and creates a more manageable, less chaotic environment. A centralized phlebotomy and sample collection center is essential.
Integration with Teaching: The OPD is where students first learn the art of clinical consultation. Consultation rooms must, therefore, be designed to accommodate a patient, a supervising consultant, and 2-3 medical students comfortably. Built-in audio-visual systems can allow for live-streaming of unique physical findings to a nearby seminar room for a larger group of students, transforming a single patient encounter into a collective learning opportunity.
3. The Inpatient Department (IPD) & Wards: The Realm of Holistic Care
The IPD is where patients stay for longer-term treatment, and its design must balance clinical efficiency with humanity and privacy.
Infrastructure Core: The modern standard is the "all-private room" model. Each room should be identical and standardized, equipped with hand-hygiene stations, a patient bathroom, a family zone, and a clinical area designed to reduce clutter and infection risk. Acoustic control is critical for patient rest. Nursing stations should be decentralized, with smaller substations located closer to patient clusters to reduce staff fatigue and improve response times.
Integration with Teaching: The ward layout must support "rounds," a fundamental teaching ritual. Corridors need to be wide enough to accommodate a team of 5-8 people without blocking clinical traffic. Each patient room should have a designated "outside-the-room" discussion area—a small nook or alcove—where the team can converse privately about the patient's care plan, allowing students to present cases and receive feedback without compromising patient confidentiality or dignity.
4. The Diagnostic & Interventional Zones: The Eyes of the Hospital
This zone encompasses Radiology (X-ray, CT, MRI, Ultrasound), Pathology (labs), and Interventional Suites (Cath Labs, Neurointerventional Radiology).
Infrastructure Core: These areas have profound technical needs: structural shielding for radiation, power redundancy for sensitive equipment, and specialized HVAC for temperature control. The layout should follow a "hub-and-spoke" model. The "hub" is the core imaging department (MRI, CT), often located centrally for easy access from the ED and IPD. The "spokes" are smaller, satellite units like ultrasound machines within the OPD pods or a dedicated CT scanner in the Emergency Department.
Integration with Teaching and Research: Integration here is both physical and digital.
Physical: Viewing rooms adjacent to CT/MRI control rooms are essential. These are soundproofed spaces where students and residents can observe live procedures and image acquisition without disrupting the technologist.
Digital: The entire diagnostic zone is powered by a Hospital Information System (HIS) and Picture Archiving and Communication System (PACS). This digital backbone allows a radiologist to pull up a scan and, with a few clicks, share it with a room full of students in the academic wing, annotating findings in real-time. This seamlessly connects a clinical finding directly to a classroom lesson.
5. The Operation Theatre (OT) Complex: The Sanctum of Surgical Precision
The OT complex is the most technically demanding and protocol-driven area of the hospital, designed around the principles of sterility and efficiency.
Infrastructure Core: The design follows a strict "sterile core" model. There is a clear, one-way traffic flow from the unrestricted zone (locker rooms, pre-op holding) to the semi-restricted zone (sterile corridors) to the restricted zone (the OTs themselves). Each operating theatre is a modular "box-within-a-box," with independent climate control and positive air pressure to prevent infection. In-built booms for anesthesia gases, power, and data keep the floor clutter-free.
Integration with Teaching: Teaching in the OT cannot interfere with sterility or patient safety. This is achieved through:
Integrated Audio-Visual Systems: High-definition cameras and microphones in the OT lights allow the surgical field to be broadcast live to an "observation gallery"—an amphitheater-style room with glass looking directly into the OT. Here, students can observe and discuss the procedure without entering the sterile field.
Adjacent Simulation Suites: The most advanced designs place a surgical simulation center immediately adjacent to the OT complex. A resident can practice a laparoscopic skill in the sim lab and then walk steps away to assist in a real case, creating an unparalleled continuum of learning.
The Connective Tissue: Integrating with Medical Teaching and Research
The true genius of a teaching hospital's design lies in the "connective tissue" that binds these clinical zones to the academic and research wings.
Physical Connectivity: Skybridges and underground tunnels are not mere conveniences; they are vital academic arteries. They allow a medical student to move from a pathology lecture to a clinical pathology lab to review a patient's biopsy slides within minutes, reinforcing theoretical knowledge with immediate practical application.
The Digital Nervous System: A unified Electronic Medical Record (EMR) is the digital lifeblood. It allows a researcher to query anonymized data for a study, a student to review a patient's full history for a case presentation, and a clinician to access all information at the point of care. This shared data platform is the most powerful integrator of education, research, and clinical practice.
The Translational Research Bridge: The physical placement of research labs is critical. They should be situated in a wing that has direct, easy access to both the clinical departments and the academic blocks. This "bench-to-bedside" proximity encourages collaboration between basic scientists and clinicians, ensuring that laboratory discoveries can be rapidly translated into new therapies and that clinical observations can directly inform new research questions.
Conclusion: An Ecosystem of Excellence
In conclusion, the infrastructure of a teaching hospital is a sophisticated, highly specialized ecosystem. Every element, from the width of a corridor to the placement of a data port, is purposefully designed to support a triad of missions: exemplary patient care, transformative medical education, and groundbreaking research. When these infrastructural elements are thoughtfully conceived and seamlessly integrated, the hospital ceases to be just a building. It becomes a dynamic, learning health system that heals, teaches, and discovers, all at once, setting the stage for the next generation of medical breakthroughs.